Executive Summary
The COVID-19 pandemic is unlike other health threats seen in the past century. From January 2020 to October 2021, more than half a million Americans died from the disease. In the event of health threats like these, an interactive system of governmental and health care actors and technologies must work together to accurately detect, report, predict and facilitate responses to prevent illness and death. This system is known as the public health data infrastructure, and public health surveillance is one essential piece of this system.
Public health surveillance enables leaders to understand where a disease has appeared and how it may spread. Through strong public health data surveillance and infrastructure systems, government leaders can protect public safety by creating policies and allocating resources based on predicted disease outbreak. One study found that if social distancing policies had started one week earlier during the COVID-19 pandemic in the United States, there could have been 700,000 fewer infections and 36,000 lives could have been saved.
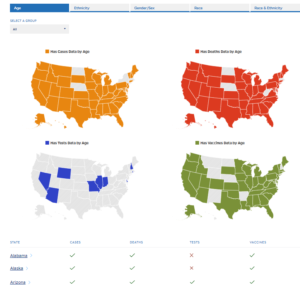
Early in the COVID-19 pandemic, the federal government struggled to collect accurate, comprehensive and timely disease data. Across federal and local government, data platforms and definitions were not standardized, which made data sharing across institutions and sectors difficult. Platforms lacked interoperability and fragmented systems negatively impacted continuity of care and efforts to aggregate large amounts of data. Nonautomated and time-consuming processes, such as the use of paper records, faxes and phone calls to share case data, affected the accuracy and timeliness of data. Finally, a lack of data use agreements and concerns over privacy and security prevented sharing information across sectors.
Many of the challenges seen at the beginning of the pandemic still affect data collection efforts one-and-half-years later. States use different definitions for a positive COVID-19 test, vaccines are not being distributed equitably and policies are not always based on public health recommendations. To help solve these challenges, the Partnership for Public Service conducted 15 interviews and one workshop with federal, state and nonprofit leaders to identify successes stories and recommendations for congressional and federal leaders. The hope is that this information will lead to substantial and rapid progress on modernizing the nation’s public health data infrastructure to improve the timeliness, quality and coordination of public health data.
This report highlights six case studies that illustrate valuable lessons learned and best practices for creating a stronger public health data infrastructure. Federal, state and academic leaders focused on workforce capabilities, technological platform decisions, data transparency and tips for creating policy.
Five key recommendations for federal leaders arose from this work:
- Invest in core public health systems.
- Ensure timely, accessible and secure data.
- Highlight public health experts as leaders.
- Standardize and define terms.
- Developing a robust, flexible and agile data workforce.
- Strengthen cross-governmental collaboration through skills trainings, report streamlining and more.
As new COVID-19 variants arise, it is more crucial than ever to invest in strong public health data surveillance and research, and to enact best practices. The Centers for Disease Control and Prevention received $500 million from the CARES Act to improve surveillance. Cross-sector partners and the federal government are well-positioned to create more robust partnerships, systems and policies to create a strong public health data infrastructure and save lives.